Shadow Health Assignments
iHuman Documentation Guide
Use this guide to help you complete documentation within the iHuman Virtual Patient Encounter. All documentation for the patient visit must be entered into the iHuman platform.
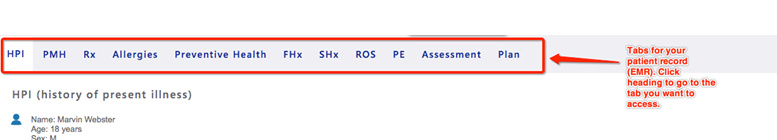
EMR Documentation

Struggling to meet your deadline?
Get your assignment on iHuman Documentation Guide done by certified MDs and PhDs in the USA. ORDER NOW!
Use the Patient Record to document pertinent information related to your history and physical exam. You are able to access and update the patient record any time while you are playing your assignment by clicking on the Show Patient Record button. Click the iHuman Documentation Guide Hide Patient Record button to return to your patient.
Include pertinent information for the focused assessment using the tabs within the EMR:
EMR tips
- Chief complaint (CC) is a BRIEF statement identifying why the patient is here – in the patient’s own words – for instance “headache”, NOT “bad headache for 3 days”. Sometimes a patient has more than one complaint. For example, if the patient presents with cough and sore throat, identify which is the CC and which may be an associated symptom
- Use OLD CARTS to document history of present illness (HPI)
- Be sure to include all past medical history, medications, and allergies.
- Include reaction/response to each allergen.
- Include dosage, frequency, length of time used and reason for use for each medication; also include OTC or homeopathic products.
- Limit preventive health, family, and social history to findings pertinent to the HPI.
- Social history may include but not limited to occupation and major hobbies, family status, tobacco and alcohol use, and any other pertinent data. Include health promotion such as seat belt use all the time or functional smoke detectors in the house, etc.
- Family history may include but not limited to illnesses with possible genetic predisposition, contagious or chronic illnesses. Reason for death of any deceased first-degree relatives should be included, for example, parents, grandparents, siblings, and children. Include grandchildren if pertinent.
- In your review of systems (ROS), address all body systems that may help rule in or out a differential diagnosis. Limit ROS documentation to positive and negative findings pertinent to focused health history. Describe findings; do not use WNL.
- Information gathered during the physical examination by inspection, palpation, auscultation, and percussion should be documented under physical exam. Limit physical exam documentation to findings pertinent to your focused assessment based on the chief complaint. If unable to assess a pertinent body system, write “Unable to assess”. Document pertinent positive and negative assessment findings iHuman Documentation Guide. Pertinent positive are the “abnormal” findings and pertinent “negative” are the expected normal findings. Separate the assessment findings accordingly and be detailed. Describe findings; do not use WNL.
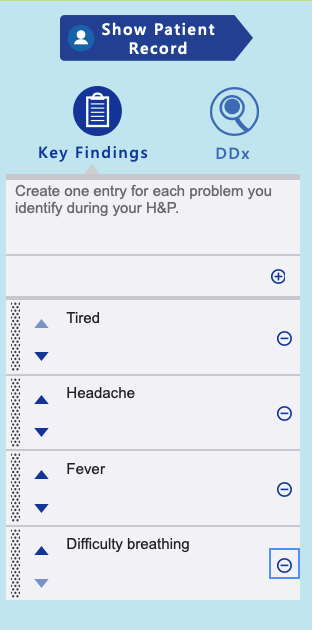
Key Findings
Add key findings at any time during your history or physical exam by clicking the + sign. Key findings may be organized using the up and down arrows. You will organize the key findings further in the Assessment step.
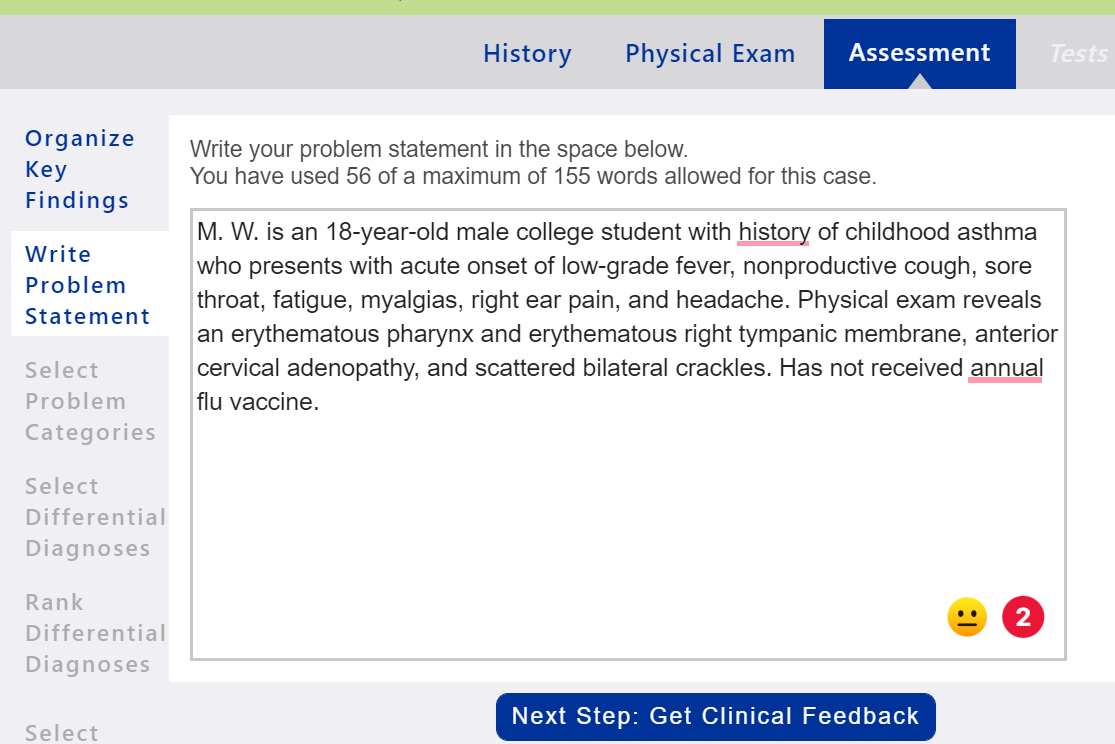
Problem Statement
Problem Statement: Document a problem statement using professional language. You will include pertinent demographic data, a brief description of the HPI and other pertinent subjective findings, and a brief description of pertinent objective findings. Use the data that you collected and documented in your EMR and summarize the data in the problem statement. Note that the problem statement has a 155-word limit. iHuman Documentation Guide A sample problem statement is shown below.
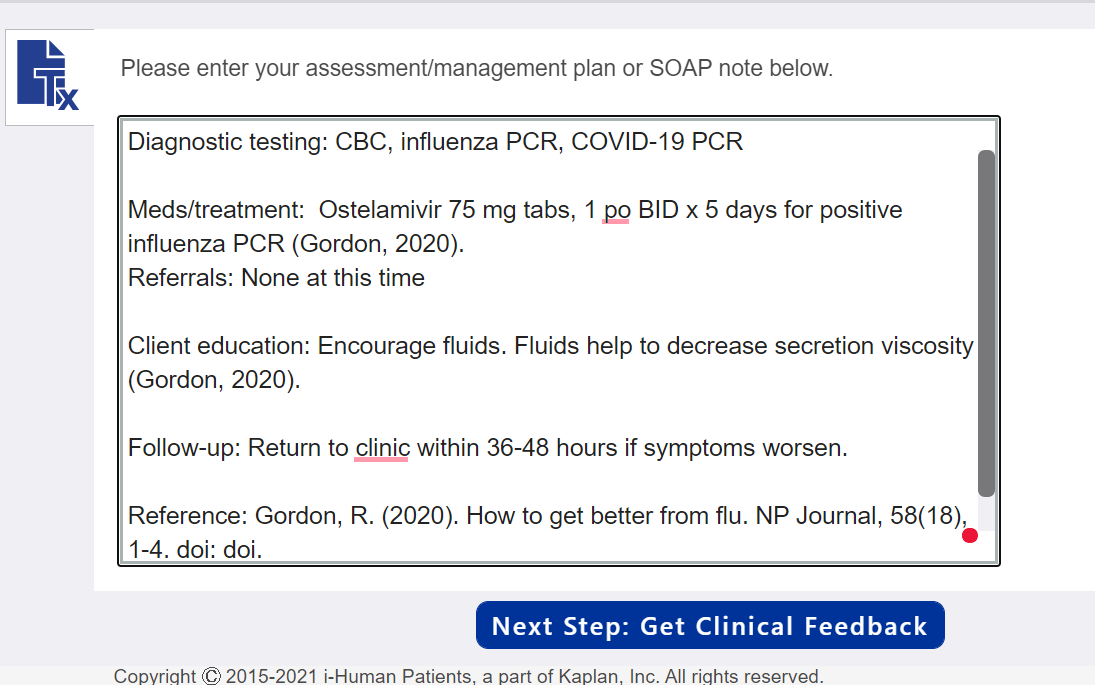
Management Plan
Using the expert diagnosis provided, create a comprehensive treatment plan using professional language. Use headings to address all 5 parts of the comprehensive treatment plan. If you do not wish to order an intervention for any part of the treatment plan, write “None at this time” but be sure to address each area. No intervention is self-evident. Provide a rationale and evidence-based in-text citation for each intervention. Include at least one appropriate, evidence-based, scholarly source to support your decisions. A sample management plan is shown below.
Management Plan Tips:
- Diagnostic tests: Appropriate tests have been provided within the iHuman case. Include the tests ordered in your management plan. Do not include results. You need not provide rationale or citation for diagnostic tests.
- Medications/treatments: List medications/treatments including OTC drugs you will order and “continue meds” if pertinent. Include appropriate, evidence-based treatment recommendations. Explain the rationale for your decisions and provide support from scholarly literature with an in-text citation.
- Consults/referrals: Provide a list of appropriate referrals. Include a rationale for each and provide support from scholarly literature with an in-text citation.
- Client education: Provide documentation of appropriate client education. Include a rationale and provide support from scholarly literature with an in-text citation.
- Follow-up: Indicate when patient should return and provide detailed symptomatology indicating if the patient should return sooner than scheduled or seek attention elsewhere.
- Be sure to include the full reference for all in-text citations used. You will not be able to use italics for the title of your journal article within iHuman documentation.
- You need only 1-2 EBP references for the SOAP note. Each reference must support your selection of interventions and guide clinical decision making. The best references are national guidelines or treatment protocols.
- You may choose to complete the SOAP note within a Word document and copy/paste to the iHuman Plan tab when complete iHuman Documentation Guide.