Shadow Health Assignments
Captain of the Ship Project – Obsessive-Compulsive Disorders
 In earlier weeks, you were introduced to the concept of the “captain of the ship.” In this Assignment, you become the “captain of the ship” as you provide treatment recommendations and identify medical management, community support resources, and follow-up plans for a client with an obsessive-compulsive disorder.
In earlier weeks, you were introduced to the concept of the “captain of the ship.” In this Assignment, you become the “captain of the ship” as you provide treatment recommendations and identify medical management, community support resources, and follow-up plans for a client with an obsessive-compulsive disorder.
Students will:
• Recommend psychopharmacologic treatments based on therapeutic endpoints for clients with obsessive-compulsive disorders “Captain of the Ship” Project – Obsessive-Compulsive Disorders
• Recommend psychotherapy based on therapeutic endpoints for clients with obsessive-compulsive disorders
• Identify medical management needs for clients with obsessive-compulsive disorders
• Identify community support resources for clients with obsessive-compulsive disorders
• Recommend follow-up plans for clients with depression disorders
To prepare for this Assignment:
• Select an adult or older adult client with an obsessive-compulsive disorder you have seen in your practicum.
In 3–4 pages, write a treatment plan for your client in which you do the following:
• Describe the HPI and clinical impression for the client.
• Recommend psychopharmacologic treatments and describe specific and therapeutic endpoints for your psychopharmacologic agent. (This should relate to HPI and clinical impression.)
• Recommend psychotherapy choices (individual, family, and group) and specific therapeutic endpoints for your choices. “Captain of the Ship” Project – Obsessive-Compulsive Disorders.
• Identify medical management needs, including primary care needs, specific to this client.
• Identify community support resources (housing, socioeconomic needs, etc.) and community agencies that are available to assist the client.
• Recommend a plan for follow-up intensity and frequency and collaboration with other providers.

Struggling to meet your deadline?
Get your assignment on Captain of the Ship Project – Obsessive-Compulsive Disorders done by certified MDs and PhDs in the USA. ORDER NOW!
Obsessive-Compulsive Disorders
Obsessive-Compulsive Disorder (OCD) is a mental health disorder that affects a person’s thoughts, feelings, and actions. Individuals with OCD often have repeated, unwanted thoughts called obsessions, and they may feel compelled to perform specific behaviors or routines, known as compulsions, to reduce the anxiety caused by these thoughts. OCD can greatly impact a person’s ability to function in everyday life, affecting their relationships, work, and emotional well-being.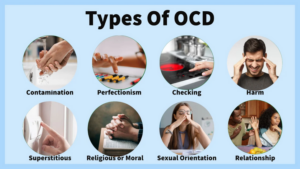
As nurses, we play a crucial role in managing the care of patients with OCD. Our tasks include OCD therapy options, providing nursing interventions for OCD, and assisting with OCD medication management. We also help implement a mental health nursing care plan that involves a mix of psychopharmacological treatments (medications), Cognitive-behavioral therapy (CBT), and support resources. This plan ensures that patients with OCD receive holistic, compassionate care.
Overview of OCD and its Impact on Patients
OCD is a chronic disorder that causes severe anxiety. The obsessions are persistent thoughts or urges, like worrying about cleanliness or safety. To reduce the anxiety, individuals perform compulsions, such as washing their hands repeatedly or checking locks over and over. This cycle can take over a person’s life.
The role of nurses in managing OCD is to assess the severity of the condition, provide care that includes both medication and therapy, and offer support to both the patient and their family. Nurses also provide information and resources about support resources for mental health patients, ensuring that those with OCD can access the necessary help, whether it’s medical, psychological, or community-based.
Creating a Treatment Plan for OCD: Nursing Interventions
A comprehensive OCD treatment plan involves using nursing interventions for OCD that address all aspects of the disorder, including the symptoms, triggers, and coping mechanisms. Nurses help create a plan that involves both psychotherapy (such as CBT for OCD) and medication. The key to success is collaboration with the patient and other healthcare providers to create a personalized treatment plan nursing.
Psychopharmacologic Treatment for OCD: Key Medications
One of the first steps in treating OCD is medication. Psychopharmacological treatments for OCD usually involve antidepressants, especially SSRIs (Selective Serotonin Reuptake Inhibitors) or SNRIs (Serotonin-Norepinephrine Reuptake Inhibitors). Medications like fluoxetine, sertraline, and clomipramine are commonly prescribed for OCD because they help balance serotonin levels in the brain, which can reduce both obsessive thoughts and compulsive behaviors.
Therapeutic Goals for Medication Management:
The main goal of using OCD medications is to help reduce the intensity and frequency of obsessions and compulsions. When patients experience fewer symptoms, they can regain control over their daily lives. It’s important to monitor for any side effects of the medications, such as nausea, headaches, or trouble sleeping. Nursing interventions for OCD should include educating patients about these side effects and working with their healthcare provider to adjust the treatment if needed.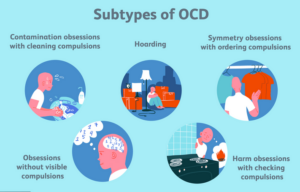
Psychotherapy for OCD: Approaches and Effectiveness
Cognitive-behavioral therapy (CBT) is the most effective psychotherapy for treating OCD. This therapy focuses on changing unhealthy thinking patterns and behaviors. A specific form of CBT called Exposure and Response Prevention (ERP) is particularly useful in OCD treatment. In ERP, patients are gradually exposed to the things that trigger their obsessions, and they learn to resist performing compulsive behaviors in response. This helps them manage their anxiety over time.
Therapeutic Goals for Psychotherapy:
The goal of CBT and ERP is to help patients recognize the irrational nature of their obsessive thoughts and reduce their compulsive actions. By doing this, they can gain control over their anxiety and reduce the impact OCD has on their lives. Individual, family, and group therapy for OCD can provide additional support and strengthen the therapeutic process.
Collaborative Care and Medical Management for OCD
Managing OCD effectively requires collaborative care in OCD treatment, which means working with other healthcare professionals, such as psychiatrists, psychologists, and primary care providers. Nurses often help coordinate care by ensuring that the patient’s medication and therapy align with their overall health needs.
Medical Management Needs:
Patients with OCD often experience other mental health conditions, such as anxiety or depression, that need to be treated alongside the OCD. This is why primary care needs for OCD are also important—patients may need regular check-ups to monitor their health and the side effects of medication. Nurses can help ensure that any additional health issues are addressed and that the patient is receiving the most appropriate care.
Community Resources for OCD Patients
Patients with OCD may face challenges that go beyond the disorder itself, such as housing or financial issues. Community resources, such as local support groups or social services, can play an important role in helping patients live well with OCD.
Community Support for OCD Patients:
- Housing and socioeconomic support: For patients struggling financially due to their OCD symptoms, support with housing, job placement, and other basic needs is essential.
- Local and online support groups: These groups provide an opportunity for patients to connect with others who understand their struggles.
- Mental health services and community agencies: Many communities have organizations that provide counseling, therapy, and other services for people dealing with OCD.
By identifying community support for OCD patients, nurses can help ensure that patients have the resources they need for both treatment and daily living. 
Follow-Up Plans and Post-Treatment Care for OCD
Follow-up care is critical in managing OCD. It’s important to monitor the effectiveness of treatment and adjust it as needed. Follow-up visits should focus on tracking progress, addressing side effects, and ensuring the patient continues to meet their therapeutic goals in OCD treatment.
Frequency and Intensity of Follow-Up Visits:
After the initial treatment phase, follow-up visits should occur every few weeks or months, depending on the patient’s progress. These visits are essential for monitoring therapeutic outcomes and ensuring that the treatment plan continues to be effective. Nurses also play a role in adjusting the OCD treatment plan nursing if necessary, collaborating with other healthcare providers to make sure all aspects of the patient’s care are managed.
Conclusion: Comprehensive Care for OCD Patients in Nursing
A successful treatment plan for OCD requires a holistic approach that addresses both the mental health and physical needs of the patient. Nurses are essential in implementing this plan, which involves psychopharmacological treatments for OCD, CBT therapy for OCD, and a range of support services. By creating a strong treatment foundation that includes medication, therapy, and community resources, we help patients manage OCD symptoms, improve their quality of life, and reduce the negative impact OCD has on their daily functioning.
Through collaborative care in OCD treatment, nurses and healthcare teams can work together to ensure that patients receive the comprehensive care they need. By coordinating follow-up care for OCD and making adjustments to the treatment plan, nurses can continue to support patients on their journey toward better mental health. Ultimately, nurses are key players in helping OCD patients manage their condition and achieve lasting therapeutic goals.

Dont wait until the last minute.
Provide your requirements and let our native nursing writers deliver your assignments ASAP.